All posts
Protesting During COVID-19

Mary McQuilkin, NP, MPH
Jun 9, 2020
6 min

COVID-19 poses a serious health threat to individuals of all ages. While older adults and people with chronic conditions such as diabetes and obesity are more likely to become seriously ill, some young, otherwise healthy people end up in the hospital too. We are still learning more every week about why some people with no health problems become very ill, and there are likely risk factors we still don’t know about.
We do know that SARS-CoV-2, the virus that causes COVID-19, is spread through the air when people talk, yell, sing, cough, or sneeze. Staying 6 feet apart from other people is helpful, and if everyone wears a mask it decreases the risk for everyone in the community.
The protests against racism and police brutality following the death of George Floyd in police custody continue across the U.S. His death ignited a powerful political movement, which is already resulting in real change to government and institutional policy. This is an important cause, and the momentum of the current movement is an opportunity for change that will not yield to the pandemic.
It is worth noting that the pandemic and police brutality and racism are interrelated issues. Black Americans are more likely to become seriously ill or die from COVID-19 due to racial disparities in health outcomes, which are caused by unequal access to services including healthcare. Black Americans also have been disproportionately affected by job losses during the pandemic. Racial injustice is a complex, multifaceted issue, but it affects all American either directly or indirectly. As Martin Luther King Jr. said, “Injustice anywhere is a threat to justice everywhere.”
If you chose to physically participate in the demonstrations, here are some pointers to help reduce the risk to your own health:

What to wear:
- A mask.
- Shatterproof eye protection: a face shield would be ideal, but you can get creative with what’s available: Do you have old ski goggles in your closet? Swimming goggles?
- Long sleeves and pants, if tolerable in the heat. Keeping your skin covered protects you from the sun, abrasions, or pepper spray.
- Comfortable shoes you can run in.
- A hat for sun protection.
What not to wear:
- Contact lenses: Tear gas in your eyes can get trapped under your contact lenses, causing further eye irritation.
- Makeup or oil-based sunscreen: Chemical irritants can stick to makeup, making it harder to rinse off your skin.
- Jewelry: Especially avoid big earrings that would cause harm if grabbed or caught on something.
What to bring:
- A bottle of water. Useful both for staying hydrated and for rinsing your eyes in case of exposure to tear gas or other chemical irritants.
- Hand sanitizer kills the virus that causes COVID-19. If you aren’t near a sink with soap and water, use hand sanitizer, especially after touching shared surfaces of a bus or train.
- A change of clothes in a plastic bag if you are able to carry a small backpack in case what you’re wearing gets covered in pepper spray.

- If you take daily medications, bring a few days’ supply in case you get arrested. Jail may require a letter from your provider with the prescriptions and a statement that they are medically necessary.
- If you have asthma, bring your rescue inhaler. If you have a history of severe allergic reactions, it would be good to bring your EpiPen.
- Menstrual pads, if needed.
Activist first aid:
Pepper spray / tear gas:
- Stay calm and leave the area; try to get upwind.
- Don’t rub your eyes.
- Use water to rinse chemical irritants out of your eyes.
- Take a cold shower as soon as you can.
- The effects of tear gas take about 30 minutes to wear off, while the discomfort from pepper spray can last up to two hours.
Rubber bullet or other projectile:
- Clean the area with soap and water.
- Apply ice for 20 minutes at a time. You can use frozen vegetables if you don’t have ice. Wrap the ice in a cloth before applying it to protect your skin.
- Elevate the injured body part when you get home.
- NSAIDs such as Aleve or Ibuprofen, or Tylenol can be used as needed for pain.

Sound cannon or long range acoustic device (LRAD):
- Run away and to the side of where the device is pointed. The sound is strongest in a straight line, so moving to the side will help.
Heat exhaustion:
- Symptoms include: dizziness, weakness, fatigue, cool sweaty skin, headaches, muscle cramps, nausea, vomiting, or diarrhea.
- Go somewhere cool out of the sun. Try to cool off by drenching clothes in cold water and removing excess layers. Drink sips of a drink and eat a small amount of a salty snack. If not recovering after 15 minutes, seek medical attention.
- Heat exhaustion can progress to heat stroke, which is a medical emergency. Symptoms of heat stroke include not sweating, hot dry skin, confusion, disorientation, and fatigue.
COVID-19 testing following potential exposure
Testing for current COVID-19 infection with a PCR test is helpful to determine if you are in the early stages of infection (pre-symptomatic), or if you are an asymptomatic carrier — a person who feels fine but can spread the virus to others. This type of test will not be positive until 5–7 days after exposure to the virus on average, so I recommend waiting about a week after protesting to come in for the swab.
The other type of test available for COVID-19, serology testing which detects IgG antibodies against the virus, is less helpful after recent exposure. Serology testing shows evidence of a past COVID-19 infection by checking your blood for evidence of your body’s immune response to the virus. This type of test takes about 2 weeks to become positive and doesn’t tell us if you may still be able to spread the infection to others (but the PCR test does). If you are interested in getting tested, schedule a COVID-19 video assessment to discuss which type of test would be best for your situation and how results should be interpreted.
Have questions about screening tests after reading news about high rates of false positive test results? Read An Explanation of the Risks and Benefits of Screening Tests. If you have read about positive and negative predictive values and want to know how these values are calculated using the prevalence of COVID-19 in a population:
Additional resources
Johns Hopkins Coronavirus Resource Center
CDC
Profiling Early Humoral Response to Diagnose Novel Coronavirus Disease

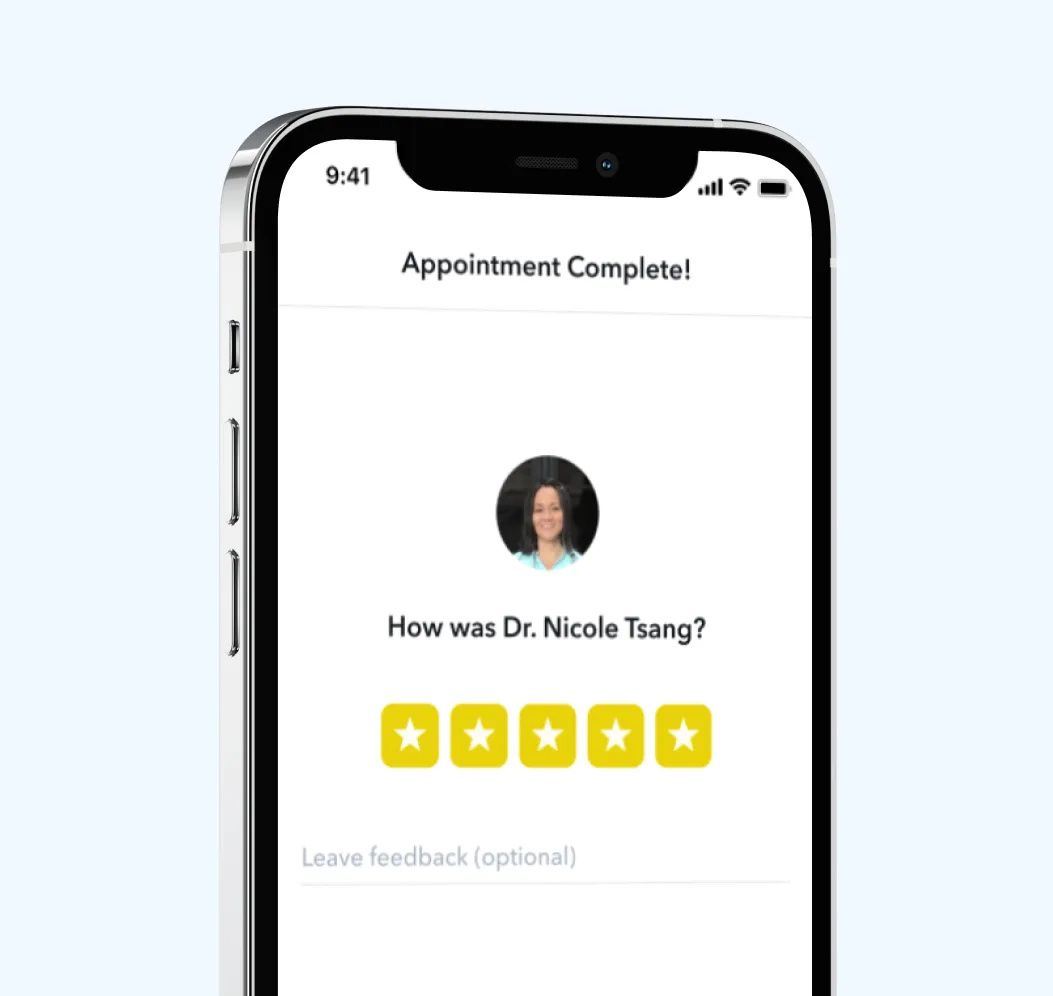
Circle Medical Providers must meet all of the following standards:
-
Exceptionally qualified in their field
-
Board-certified
-
Deeply empathetic for patients
-
Follows evidence-based care guidelines
-
Embracing of diverse patient backgrounds
-
Impeccable record of previous care
400+ Primary Care Providers.
100% Confidence.
No matter which Provider you choose, you will be seen by a clinician who cares deeply about your health and wants to help you live your happiest, healthiest life.
Circle Medical Providers are held to an exceptionally high standard of compassionate, evidence-based care.
Book Appointment